by Michael Wong, JD (Executive Director, Physician-Patient Alliance for Health & Safety)
There is a need to improve rapid response teams and code blue activations. 50% of Code Blue events involve patients receiving opioids. Moreover, unrecognized postoperative respiratory failure that results in cardiopulmonary arrest is a daily occurrence at healthcare facilities across the United States.
In a recent interview with the Physician-Patient Alliance for Health & Safety (PPAHS), Eyal Zimlichman, M.D., MSc., spoke at length about improving rapid response teams and code blue activations.
Dr Zimlichman holds dual appointments as Deputy Director General and Chief Quality Officer at Sheba Medical Center in Israel and at the Center for Patient Safety Research and Practice at Brigham and Womenâs Hospital and Harvard Medical School
The success of rapid response team deployment and Code Blue activations is hugely dependent on timing – the earlier patient deterioration is identified and acted upon, the sooner intervention may take place. Dr. Zimlichman spoke about the need for early detection and intervention:
⦠mostly in general floors, we have intermittent vital signs checks. These checks would go and somewhere between every six hours or even eight hours or sometimes four hours, but certainly not continuousâ¦
So by the time of intervention between one vital sign check to the other, we actually would get to the patient bedside only when he goes into cardiac arrest. If that deterioration occurs. So being able to continuously monitor patients on general floors, much like we do on ICUs, could be something that would make a significant contribution to preventing these preventable deaths inside hospitals.
Dr Zimlichman says that continuous electronic monitoring of patients holds the key to improving early detection and intervention:
⦠I think that’s a common notion today among the experts that continuous monitoring is what we call the missing link to making rapid responses to the work â¦
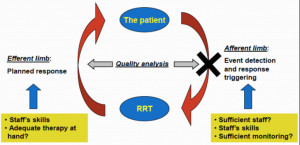
[Research has] shown that hospitals have implementation of rapid response system have not shown an improvements in outcomes, have not shown a decrease in mortality that we were aiming to see. And there is always that question, why is that the case? And if we look closely into rapid response systems, we know that there’s an efferent and an efferent we’re mainly saying that there is first of all, understanding that there’s a need to activate the team and then once we understand that there’s the actions that the team take â¦
[Using the continuous monitoring system in our research] there’s a 50% chance that [when the alarm sounds] this patient would need an ICU. When the nurse gets that alert on top of her clinical judgement, it reinforces her decision making and I think that factor alone contributes to a better and efficient activation of the system.
To listen to the complete interview with Dr. Zimlichman, please click here.
For another interview with a clinician who has been able to reduce the need for rapid response activations by more than 50%, please click here.